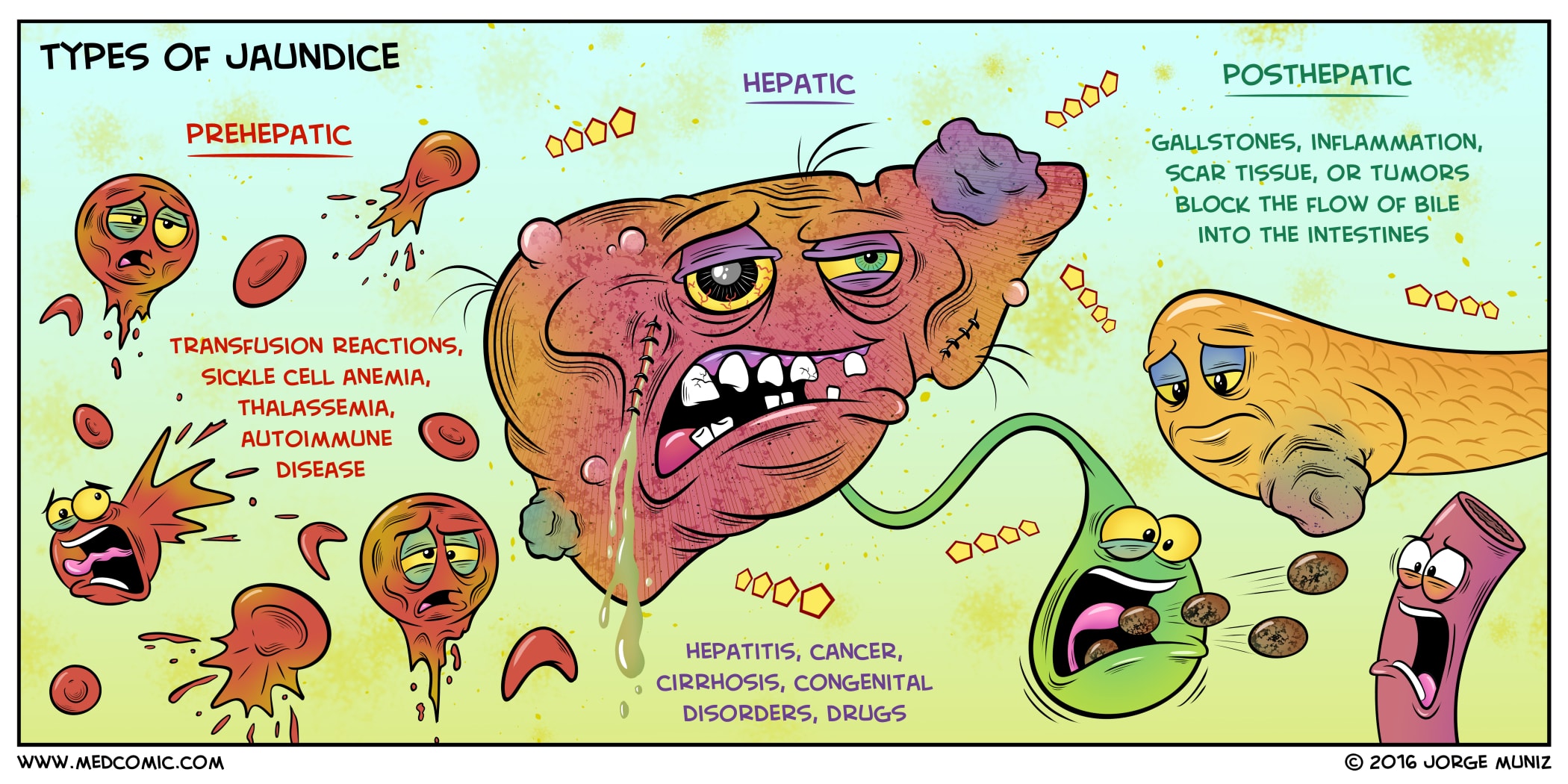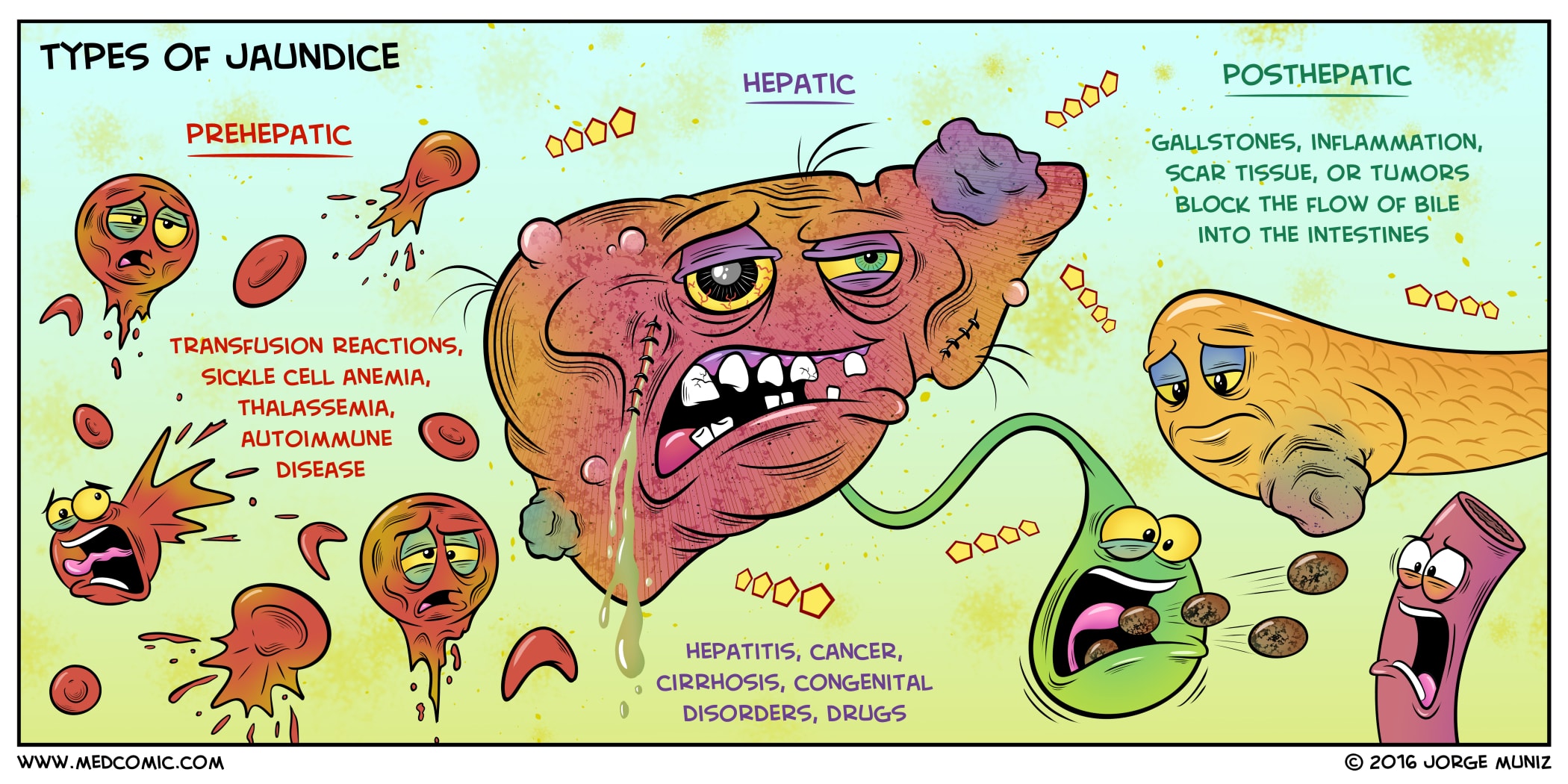
(Above image from Medcomics by Jorge Muniz, PA-C)
Ms. B is a 56-year-old woman who comes to your office because her skin and eyes have been yellow for the past 2 weeks.
Ms. B also tells you she has dark urine, light-colored stools, anorexia, and fatigue. She has no nausea, vomiting, abdominal pain, or fever. Ms. B’s physical exam shows scleral icterus and jaundice as well as hepatomegaly, with her liver edge palpable 7 cm below the costal margin. The liver extends across the midline, and the spleen tip is palpable. There is no abdominal tenderness or distention. There is no peripheral edema, and the rest of her exam is normal.
Given the pivotal historical points (dark urine and light colored stools) and the physical exam findings of jaundice, hepatomegaly, and splenomegaly, you are confident that Ms. B has hyperbilirubinemia and suspect that it will be primarily conjugated. You obtain the following initial tests: total bilirubin, 13 mg/dL; direct bilirubin, 9.6 mg/dL; AST, 250 units/L; ALT, 113 units/L; alkaline phosphatase, 503 units/L; albumin, 2.8 g/dL; prothrombin time (PT), 15.4 s (control 11.1 s); WBC = 22,000 cells/mcL with 80% PMNs, 16% lymphocytes, and 4% monocytes. The platelet count is normal.
Ms. B had a blood transfusion in Latvia in 1996. She has no history of injection drug use, tattoos, or smoking, but she has consumed between 2 glasses and 1 bottle of wine daily for years. Her past medical history is notable only for Helicobacter pylori–positive gastric and duodenal ulcers 6 years ago, treated with eradication therapy. She is taking no medications.
Ms. B’s transaminases are consistent with, but not diagnostic of, ALD. An imaging study is necessary not to rule in ALD but rather to exclude alternative diagnoses. As discussed in Chapter 3, Abdominal Pain, ultrasound is the best first test to look for stones in the gallbladder, although the sensitivity is less for common bile duct stones. However, in this patient, pancreatic cancer or other malignancies are more likely causes of extrabiliary obstruction than stones; therefore, an abdominal CT scan or MRCP would be a better first test. Tests for hepatitis are necessary in all patients with liver disease and are especially important in Ms. B because of her history of a blood transfusion.
Ms. B has an abdominal CT scan, which shows an enlarged, nodular liver, moderate ascites, and a normal pancreas. Her ANA, hepatitis A IgM antibody, HBsAg hepatitis B IgM core antibody, and hepatitis C antibody are all negative.
SOAP Note:
S: Ms. B is 56 y/o female patient c/o “yellow skin and eyes” x 2 weeks. Reports darkened urine, clay-colored stool, anorexia and fatigue. Denies nausea, vomiting, abdominal pain, or fever. Denies history of IDU, tattoos, or tobacco use. Admits to average of 4 glasses of wine daily for years. Reports history of H. Pylori-positive gastric and duodenal ulcers 6 years ago and 1 blood transfusion in 1996.
O: Physical exam reveals scleral icterus, jaundice, and hepatomegaly. Liver edge palpable 7 cm below costal margin. Spleen palpable. No ABD tenderness or distention. No peripheral edema. Rest of physical exam unremarkable.
A: Patient is experiencing conjugated hyperbilirubinemia as evidenced by jaundiced appearance and dark urine. Clay colored stool indicates that there is either an intrahepatic or extrahepatic disruption in the conduction of bile to the duodenum. Suspected Alcoholic Liver Disease (ALD) or hepatitis.
P: Order Aspartate Aminotransferase Test (AST) to test for blood AST levels and abdominal CT scan to assess for extrabiliary obstructions. Order compulsory full Hepatitis panel secondary to history of blood transfusion. Educate Mrs. B about the long-term effects of alcohol consumption and liver disease as well as serious risks associated with drinking. Develop plan with Ms. B to reduce her alcohol consumption and schedule follow-up in 2 weeks to check on progress of her condition and confirm reduced alcohol consumption.
Write-Up Topic: A Heuristic Approach to Developing a Differential Diagnosis of Hyperbilirubinemia
A patient that presents with jaundice has elevated bilirubin in their bloodstream. The first question that must be answered is, “Which kind of bilirubin is the main culprit?”
There are two major categories of hyperbilirubinemia: conjugated and unconjugated. This is tested for as either more than 50% “direct” or “indirect” in our blood, respectively. All bilirubin, as it’s been freshly released from lysed RBCs, originally circulates as unconjugated until it is processed by the liver into conjugated bilirubin. The conjugated bilirubin is converted into bile, carried to the duodenum via the biliary tract, and excreted in our stool, giving our stool it’s characteristic medium to dark brown color. Some bilirubin will interact with the microflora of our intestinal tract and be reabsorbed into our blood. Most of that reabsorbed conjugated bilirubin will be reabsorbed by the liver and turned back into bile, but some will be filtered by the kidneys. Alternatively, if conjugated bilirubin is not being converted into bile, or the bile is not making its way to the duodenum, it will become backed-up in the liver and ultimately back into the bloodstream and ending up in the kidneys. If there is enough conjugated bilirubin in circulation, it will eventually become concentrated in the urine enough to darken the color from amber to light brown.
Why am I spending so much time on urine and stool?
Jaundice with normal urine and normal stool indicates that liver function and bile conduction are intact, but that there is still a massive influx of circulating, unconjugated bilirubin secondary to major hemolytic events.
Jaundice with dark urine and light stool indicates that conjugation by the liver is intact, but for some reason it is not making its way to the intestines as bile. This could be due to occlusion, internal or external, of the biliary tract or something internal to the liver that is prohibiting the full production or conduction of bile such that that conjugated bilirubin is backing-up into the bloodstream.
These are a few examples of the ways in which we can start to build a reliable foundation upon which to build our differential diagnosis just from an effective HPI and PE. We will still send out for serum bilirubin testing to determine the percentage of conjugated versus unconjugated bilirubin, but we can already get a sense of which pertinent negatives need to be ruled out and which kinds of tests should be ordered without wasting time or resources.